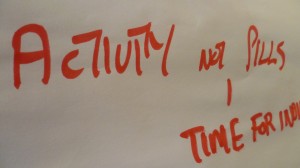
Darnall Wellbeing: “There are other ways to stay healthy”
Overview
- Darnall Well Being (DWB) is a local, not-for-profit, community health organisation working to help the people of Darnall, Tinsley and neighbouring areas in Sheffield stay healthy.
- We offer a combination of activities, 1to1 support and volunteering opportunities as well as deliver local health campaigns, health events, brief-intervention training and talks.
- Our greatest asset is the empathy of our local infrastructure of volunteers and staff – support from next door.
- Through our integrated programme of activities and services, we aim is to reduce health inequalities by helping people build their knowledge and resilience to manage their own health and wellbeing.
How do we help to building community wellbeing, resilience and social capital?
Key point is that it isn’t one thing but a combination of interconnected factors.
- Our services help to remove barriers, are culturally sensitive where appropriate, build trust, listen and respond to local need and are underpinned by our volunteers.
- We nurture an environment where individuals can be:
- in control of their own lives, able to understand and help themselves and others
- socially connected: feel like they are part of something
- confident: have a role to play
- have the right knowledge and access to support at the right time in order for them to be both emotionally and physically resilient: the ability to cope with life.
Our approach is:
- collaborative, people are part of the process, partnerships and links – we bring different people, cultures and groups together with a shared purpose
- consistent, ongoing core programme is prioritised
- client-led, support for people to set and maintain their own goals
- we raise awareness of and increase access to services and build connections to help mitigate risks such as lonliness, isolation and depression and therefore a community and individuals can become more resilient:
Improved mental health, less likely to become ill and know where to ask for help.
Current Provision 2015:
 Core Activity Programme
Core Activity Programme
- Health Walks Programme(weekly, monthly, women-only and trips)
- Tai Chi, Craft & Gardening Group, Reading Group
- Women’s Health Groups (gentle exercise and health advice, Somali Dance)
- Men’s Health Groups (gym, 5-a-side football, healthier lunch club)
- Slovak Roma Outreach Youth Activity (football, crafts, dance)
- Health Awareness Campaigns, Events & Drop-Ins, Consultation
- Conversation Club, Cook & Eat Sessions, Learn to Ride sessions with Pedal Ready
- EU Monthly Drop-In & Signposting
- Social Prescribing
A signposting service via GP Referrals for 1:1 advice from a skilled person who understands what will be helpful, is able to link someone to local services and has some understanding of the psychosocial aspects of health.
- Health Trainer Support Service
Health trainers are non-clinical staff that works with people to develop a health plan and encourage positive behaviour change around diet, healthy eating, exercise, diabetes management or chronic pain.
- Health Champion Volunteer Programme
DWB has around 40 active volunteers at any one time. Health Champions (HCs) are local volunteers who are engaged, trained and supported to promote positive health messages and inspire and help their friends, families, neighbours and colleagues to lead healthier lifestyles. The programme not only helps raise health outcomes for the community but also positively impacts on the volunteer through increasing skills, confidence and employability.
We now also run a Pregnancy & Early Programme, with bespoke training for volunteers to be able to support pre and post natal families and children up to 2 years. Link are made to local baby clinics and referrals through family support, dulas, midwifes and health visitors.
Examples of Health Campaigns, Pilot Projects and Partnerships:
- Warm Homes Healthy People
- Cancer Awareness Outreach
- Eat Well Project – community research, Oct 14 – Mar 15
- One Darnall – Roma Slovak Community Workers, Oct 14 – Mar 15
- Roma Health Project – Prime Minister’s Challenge Fund, Jul 15 – Jul 16
- Practice Champions, Nov 2013 – Mar 2016
- Work with key local groups and networks e.g. older people and BME groups such as Somali, Pakistani, Bengali and Slovak Roma, neighbourhood fora Drugs & Alcohol Coordination Team
Enhanced Primary Care
DWB and the Clover Group Practice – a new model of building individual and community resilience and changing the way primary care is delivered.
DWB took up tenancy in Darnall Primary Care Centre (DPCC) in May 2013, shared with other services (Physio, GPs, Neuro-enablement, Health Visitors, District Nurses) and has been working closely with Clover Group to develop a new model of building individual and community resilience and a programme of joint work which will make a significant contribution to delivering CCG Priorities: improved care planning and reducing emergency hospital admission and A& E attendances. DWB will offer an enhanced support package and manage, co-ordinate and promote self-care, empowering patients to manage their own health. DWB has a very strong track record of delivering this work
DWB and Clover Group are developing and testing new ways of working (as well as the Practice Champions project outlined above), including a new care planning model which shifts much of the decision making and care planning for particular patients away from clinicians to skilled, experienced Health Trainers from the local community.
The Health Trainers will not make clinical diagnosis/treatment decisions, but because they understand and are trusted by the community are better able in some cases to work directly with patients to improve their self care.
There are several voluntary organisations in the city providing Health Trainers and Health Champions, but this model is radically different because the community organisation and the Health Trainers work as part of the practice team, not an external end referral point for clinicians to refer or signpost patients as and when they feel necessary.
Enhanced Primary Care – Health Trainer client Case Study
Client: Hazel 82 (White British).
Nature of the health need:referred by her GP for the following reasons:
- To lose weight
- Borderline diabetes
- High cholesterol
- To eat more healthily, reduce portion size and eat the right type of foods
Change in behaviour (April 2012- May 2015):
- Started attending Monday walk and Thursday women only walk.
- Started with smaller plate sizes and eating more fruit and vegetables.
- Halved alcohol consumption.
- Referred to the South Yorkshire Energy Centre for warm homes discount scheme to receive £130 off next electricity bill.
- Became Health Champion volunteer, achieved over 360 hours of volunteering.
- Had positive contact with 60 beneficiaries in first year of volunteering, which is now over 100 beneficiaries.
- Went on social trips with the Family Development Project
- Attended Introduction to Community Development and Health course.
- Made new friends locally from various different cultures and backgrounds..
Patient perspective:
I was recommended to attend Darnall Well Being about 3 years ago or more by my Doctor’s surgery as I was a little overweight, had high blood pressure and high cholesterol and was borderline diabetic. I didn’t want to take statins so took their advice. I was introduced to a Health Trainer and followed their advice and managed to get myself fit.
We were asked if we would like to become volunteer Health Champions, our main duties are acting as receptionists one morning a week on the Well Being Enquiry Desk. I find this interesting as we are trying to attract people of all cultures to take part in various activities and to mix with people of all nations. This, I have seen happen and overtime have got people mixing and enjoying a laugh together and socialising.
This to me is giving more quality to life and making me feel happier, healthier and more satisfied with my own life. It has also given me more confidence in life and can listen to other’s problems and as they say “a problem shared is a problem halved”. I have made new friends of all cultures and feel healthier, may this develop further into bigger things.
Having friends and being useful in the community really helped me when my partner passed away earlier this year. By keeping active and keeping my mind going I haven’t had time to feel sorry for myself. I have kept a positive outlook on life.
Volunteer Development Worker perspective:
When we first met Hazel she was feeling depressed and very unhappy with her health. She felt less needed because the grandchildren didn’t need her as much. She didn’t want to take statins so wanted to improve her health with local support.
Helping with the women only walk has led Hazel to have a really positive attitude towards the needs of other nationalities and people. She says that even with the different languages she finds a way to communicate and share experiences. Hazel lives alone so her social network is fundamental to her wellbeing. Her confidence and health have improved dramatically to the extent that she can now lead the walk. She has maintained positive changes in her lifestyle even when faced with new challenges and has inspired others to make healthy changes.
She has continued to volunteer with Darnall Wellbeing and introduced her friend to the project too. They have been able to volunteer together and support each other. Through the social prescribing tools that Hazel uses on the Enquiry desk she has found out more about the help available for disabilities and adaptations in the home. She has also joined Age Concern. She has benefitted from a lot of information from training with other
volunteers such as support for Alzheimer’s dementia, which affects a couple of her friends, and about cancer awareness.
At 82 years of age Hazel is a great example of taking care of your self and active citizenship. Even through the loss of her partner she has maintained her health and wellbeing and social life to live life to the full.
Aileen (left) and Hazel (right) at the Enquiry desk at Darnall Primary Care where the signpost local people to services and activities that help promote their wellbeing.
Enhanced Primary Care – Health Trainer client Case Study
Client: Richard, aged 44 (White British male).
Nature of the health need:
Richard was referred by his GP for the following reasons:
- To lose weight and walks with the aid of a stick
- Poor diabetic control (blood glucose level 109mmol)
- To encourage him to take part in DESMOND and to increase understanding of disease.
- To eat more healthily, reduce portion size and eat the right type of foods
 Change in behaviour (April-June 2014):
Change in behaviour (April-June 2014):
- Richard has started to attend Ponds Forge Gym and go swimming (through Exercise Referral)
- Attended DESMOND and enjoyed it and learned a lot from it, “it was really educational”.
- Started with smaller plate sizes and eating more fruit and veg
- Referred to the Community Support Worker and Weigh Ahead
- Using the Shortened Warwick-Edinburgh Mental Wellbeing Scale, Richard now often feels optimistic about the future, feels useful, feels close to other people and been able to make up his own mind about things. Whereas before, it was none of the time or rarely
Patient perspective:
“It started with the GP, who referred me because I’m trying to lose this weight and eat the right type of foods. You’ve actually opened my eyes to a lot of things I didn’t know.
The difference is I was lazy. I was sitting in the house eating all the wrong things; eating crisps and chocolate. With me being a diabetic I’ve got to eat healthier and with coming to Darnall Well Being (DWB) it has kick-started me in to starting to eat healthy again.
You also put me in the direction with referrals to the community support workers and places I didn’t know I could get help, all from yourselves.
There are a lot of things that I was unable to do because of my disabilities, especially my weight. DWB has actually open doors and it’s set my mind in to action.
It’s good having DWB involved in the actual surgery. It doesn’t just feel all clinical. You’ve got yourselves –It’s like talking to a mate, a friend. You are so friendly, it’s unbelievable. I daren’t tell my GP everything. I hide a lot from them and I can open up to you. This feels like a community centre coming here, not like a GP surgery. It’s not a magic tablet. You have actually taken me out of the gutter, got me on the path and I’m following that path and I’m trying not to fall back in to the gutter.
I’m wanting to naturally lose this weight because at the end of the day, if I can’t lose the weight I’ve got to have a gastric band, which I’ve got a 50/50 chance of coming out from because of my diabetes being a rack. My doctor’s happy with me though; I’ve lost a stone.”
Enhanced Primary Care Case Study
Health Trainer (Yvonne) Client: Mohammed, aged 86 (South Asian Male).
Overview:
Patient attended his first appointment in Feb 2014 at the surgery. Home visits were agreed for future appointments because he struggled to climb the stairs.
Nature of the health need:
- Diabetes
- In remission from Lung cancer
- Dementia
Agreed Personal Health Plan (PHP):
- Manage diabetes with healthy eating – increase intake of fruit and vegetables
- Monitoring his blood glucose level with home kit
- Apply for Sheffield City Council – minor works grant
- SCC – CSW support
Patient’s main focus:
- Manage diabetes
- Get information/support to apply for blue badge
- Be comfortable at home – keeping warm in winter months
- Patient engaged in the service and asked relevant questions about Diabetes and his health and felt he was doing ok at home to monitor his blood glucose level.
- He expressed concerns about the draught form his back and front doors and the difficulties with keeping warm in the winter even with central heating and a gas fire.
Background – Family relationship
Mohammed lives with his wife and she is his main Carer. Prior to his referral to DWB he would normally attend his appointments at GP surgery and hospital if necessary
He often talked about his family, not being able to see his grandchildren and not remembering where he put things in the house. His wife expressed her sadness and the strain on their relationship because she found it difficult to cope and she had no support. She did not feel able to get some time on her own because Mohammed needed constant care.
He often complained of chest pain when he had to use the bathroom because of the low sink and toilet due to his height. Prior to the referral, he had difficulty climbing the stairs to use toilet upstairs due to reasons stated above. She agreed to implement a system whereby he used a bucket down stairs. He spends all his time downstairs and has a bed downstairs where he sleeps at nights. He felt restricted to downstairs and complained about the cold and draft from the doors.
His gas bills were high, but since he got a new back door it is less draughty in the kitchen. He used the £2000 grant towards the back door and the bathroom.
Outcome
- He was awarded the SCC Minor Works Grant which he used to replace his back door. He also changed the toilet and basin in his bathroom which made life easier for hi. The original ones were too low for his height and he had difficulties with them, for example he had to bend low to wash his face and it cause pain to his lungs.
- I referred him to SCC Community Support worker. She liaised with SCC Adaption & Equipment Team and supported patient to choose a suitable builder to carry out the necessary work required in meeting the criteria for the Minor works grant
A Community Support Worker also worked with the patient on the following
- Disabled parking permit – his wife owns a car and it would be a big help when she accompany him to hospital appointments etc.
- Depart of Work and Pensions – assessment to check if patient is entitled to any other benefit or is on the right benefit to claim a higher rate of disability allowance.
Patient talked about forgetting things and agreed to attend his appointments for some memory/dementia test/scan.
Patient perspective:
The Council Grant has been successful and I got a new back door. No more draught and water coming in, new toilet to make life more comfortable for me. I will use some of the money for some work that will be carried out to the electrical meter board.
Wife’s perspective:
- He is in less pain and doesn’t rely on me as before to assist him in bathroom, toilet and basin are to his height now
- Gas bills not as high, a bit warmer downstairs but front door needs changing
- Goes up stairs only night now and managing better going upstairs
Follow up
- Client has been diagnosed with Dementia and received Dementia pack from Sheffield Alzheimer society.
- He has agreed to attend DESMOND to learn more about managing diabetes.
- He was visited by DWP and awaiting their reply about higher rate disability
- His blue badge application is on going
- Government scheme – free insulation for his cellar
