How has Covid-19 – and the associated lockdown measures – affected mental health and wellbeing in the UK?
Downloads

The quick read: what you need to know
- Anxiety and depression increased in the UK as the Covid-19 pandemic took hold, with people’s mental health affected by both adverse experiences regarding their health, jobs and finances as well as worries about what might happen in the future. Anxiety and depression have fallen since the highs seen at the start of lockdown but remain above pre-pandemic levels.
- Anxiety and depression have been highest among young adults, those living alone, those living in urban areas, and people with lower household income, with children, and with a diagnosed mental illness.
- How we spend our time is important for our mental health. Outdoor exercise and gardening can improve our mental health, while spending too much time following the news can be harmful.
Mental health, wellbeing, and Covid-19
How we feel about our health, both mental and physical, is one of the most important determinants of our subjective wellbeing. National data identifies the number of people whose mental health has been affected by the pandemic.
- According to ONS data, when the lockdown started at the end of March, 49.6% of people reported high levels of anxiety, compared with just 21% in the last quarter of 2019. By August, this had fallen to 30%.
- Almost one in five adults (19.2%) were likely to be experiencing some form of depression during the Covid-19 pandemic in June 2020; this had almost doubled from around 1 in 10 (9.7%) before the pandemic (July 2019 to March 2020).
- One in eight adults (12.9%) developed moderate to severe depressive symptoms during the pandemic. A further 6.2% of the population continued to experience these levels of depressive symptoms, while around 1 in 25 adults (3.5%) saw an improvement between March and August.
The increase in mental health problems since the start of 2020 is unsurprising given the profound impact that Covid-19 has had on many people’s lives. Data collected by the Covid-19 Social Study from over 70,000 people has shown how mental health has been affected since March 2020 and identifies the risk factors that policymakers and practitioners should recognise in their efforts to support people’s mental health. This briefing summarises findings from this study.
How does mental health relate to wellbeing?
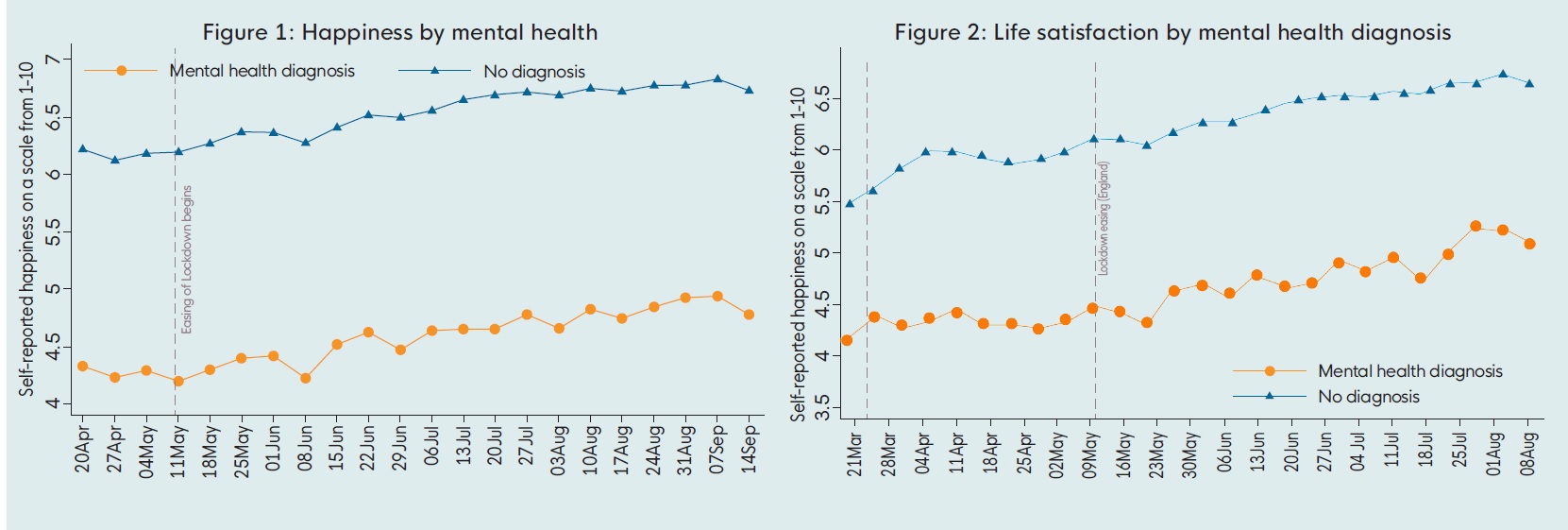
Mental health and personal wellbeing are closely related but distinct. People with diagnosed mental health conditions are more likely to have a lower level of self-reported wellbeing as measured by subjective questions on, for example, life satisfaction and happiness. (See Figures 1 and 2) However, this is not always the case as an individual’s wellbeing is influenced by a wide range of other factors besides mental illness, such as physical, financial and social issues.
Certain factors can influence mental health and wellbeing independently. For example, while children with special educational needs are more likely to experience mental illness, such needs do not necessarily impact their wellbeing.
Figures 1 and 2: People with a mental health diagnosis have reported statistically significant lower levels of happiness and life satisfaction. Data collected from the Covid-19 Social Study, April – September 2020:
Covid-19 worries and experiences affect mental health
The Covid-19 Social Study asked participants to report what factors in the prior week had caused them minor and major stress, defined as stress that was constantly on their mind or kept them awake at night. Results confirmed that the pandemic has had real and tangible effects on people’s health, employment status, social lives and relationships, which we know can negatively affect mental health and wellbeing.
But the study also showed that worrying about these adversities and the risk of them occurring can also be a cause of anxiety or depression.
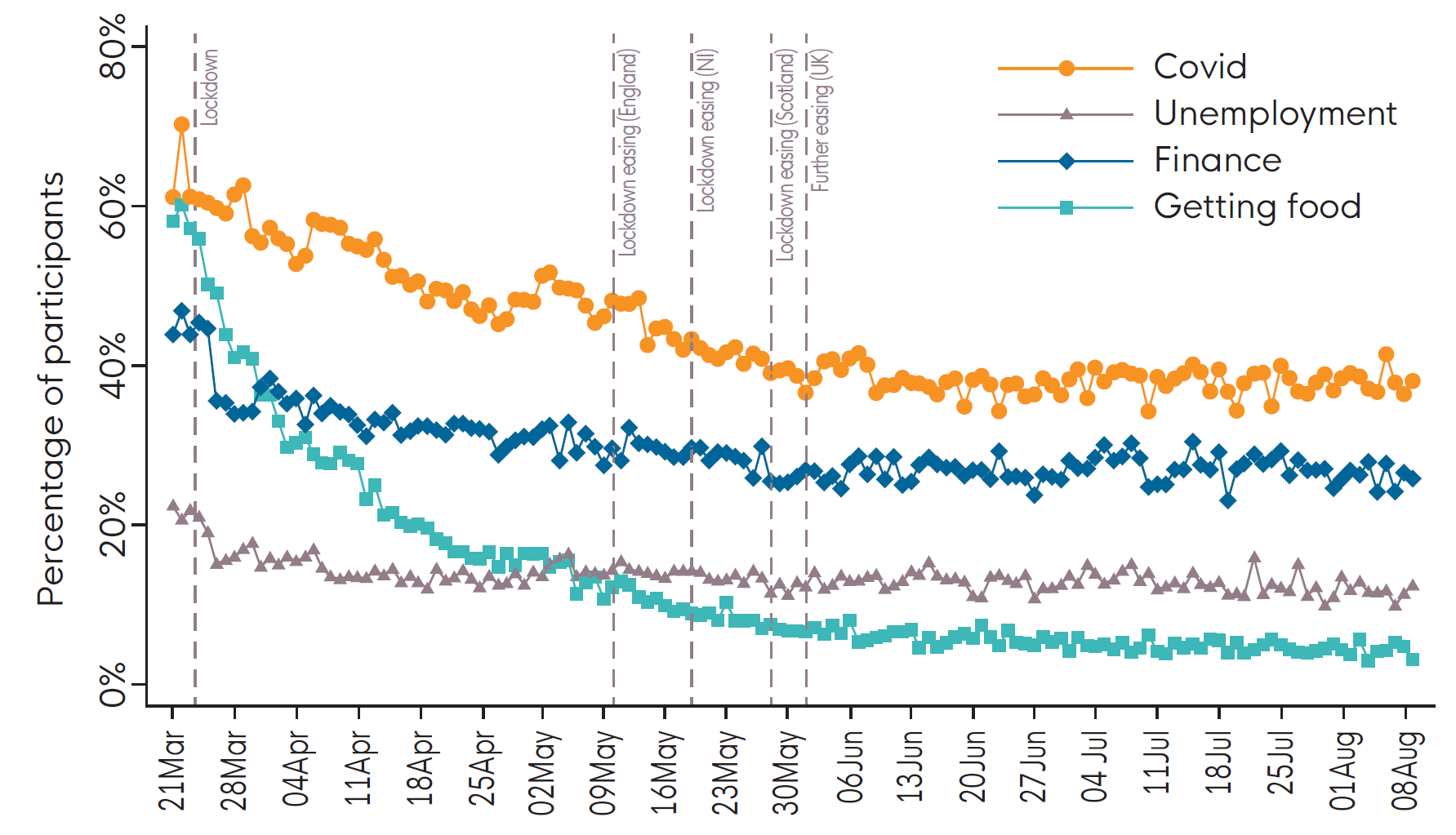
Figure 3: The study captured worries and experiences related to Covid-19 illness, financial difficulty, loss of paid work, difficulties acquiring medication, difficulties accessing food, and threats to personal safety. Anxiety was measured by the Generalised Anxiety Disorder Assessment (GAD-7 ) and depression was analysed using the PHQ-9 Patient Health Questionnaire.
Sources of stress
Stress relating to catching Covid-19 and becoming seriously ill from Covid-19 was the most prevalent stressor, worrying 40% of people. Worries about finance, affecting one in four people, and unemployment affecting one in six, stabilised by August despite the end of furlough schemes and more companies discussing redundancy measures. Worries about accessing sufficient food affected around one in 20 people and has remained a residual worry. People with diagnosed mental illness have been more worried about all factors.
Analysis of the Covid-19 Social Study data found that:
- The more worries and adverse experiences people had, the more anxious and depressed they were.
- Adverse experiences had a bigger impact on anxiety and depression for people with lower socio-economic status.
- Different types of adverse experience had a different impact on people’s mental health:
- Adversities relating to accessing food, accessing medication, and personal safety were associated with higher levels of anxiety and depression
- Adversities relating to employment and finance were not associated with changes in mental health.
- Worries about changes to employment and finance did affect people, which may have decreased mental health in the lead up to the event such that people were already at a floor level of mental
health by the time the actual event occurred. - Experience of COVID-19 symptoms was only related to higher depression scores.
Both the total number of worries and adversity experiences were associated with lower quality sleep. Each additional experience was associated with a 1.16 times higher odds of poor quality sleep, and each additional worry was associated with a 1.20 times higher odds of poor quality sleep. All worries and experiences were significantly related to poorer quality sleep except experiences relating to
employment and finances. Having a larger social network offered some buffering effects.
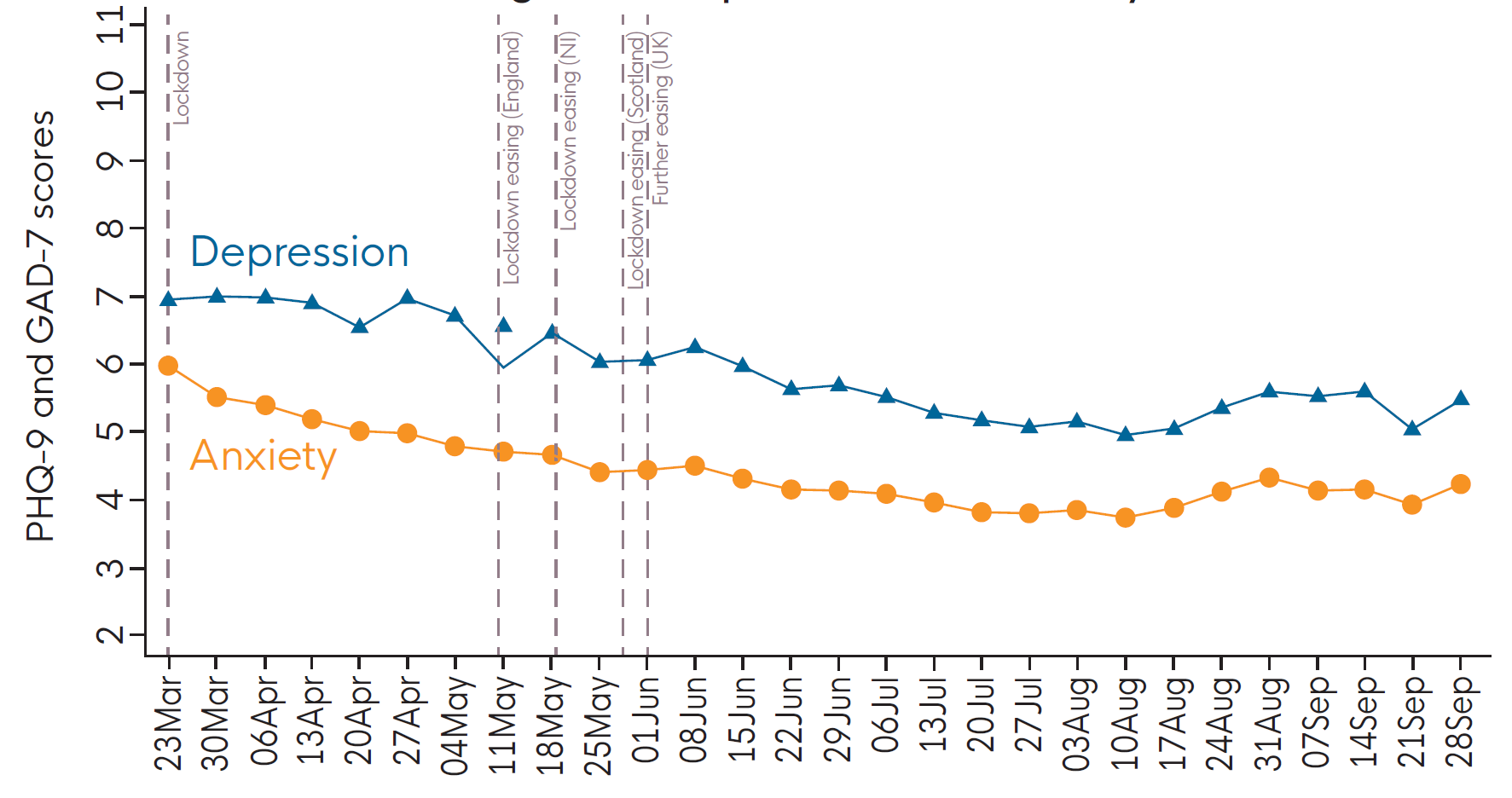
Depression and anxiety fell during lockdown, but may be rising now
Over the first two months of lockdown, there was a decrease in anxiety and depression amongst participants as a whole, and levels continued to fall in the UK from April. However, overall levels remain higher than pre-pandemic reported averages using the same scales. As we move into the next phase of the pandemic, depression and anxiety levels are beginning to rise again.
How Covid-19 has affected groups differently
Depression and anxiety are highest among people who:
- are young adults
- have a lower household income
- have a diagnosed mental illness
Depression and anxiety are also highest among people who live:
- alone
- with children
- in urban areas
The Covid-19 Social Study also looked specifically at vulnerable groups and identified those most likely to experience moderate or severe depressive symptoms during the pandemic. These include those with:
- Psychosocial and health-related risk factors, including pre-existing physical and mental health conditions, experience of psychological and/or physical abuse, and low social support.
- Low socioeconomic position, identified based on a composite score that included low household income, employment status, education, household tenure, and household overcrowding.
Implications for a wellbeing-based recovery
The mental health of people in the UK was a concern prior to Covid-19 pandemic which saw depression and anxiety levels spike. They have not yet fallen back to pre-Covid-19 levels, which were already too high and negatively impacting the wellbeing of the UK population.
Even before the pandemic hit, scaling up the treatment of mental health illnesses was highlighted as a powerful and cost-effective way to improve wellbeing in the UK. A recovery plan could usefully include strategies to:
- Support and restore access to mental health services. Particularly for the those with pre-existing mental health issues and those out of work.
- Invest in activities that support people’s mental health, particularly those that have been helpful in recent months, such as outdoor activities and exercise, which will be less accessible but just as crucial during upcoming winter months. Encouraging people to spend less time following news about COVID-19 may also help to prevent declines in mental health and wellbeing.
- Research and develop interventions for younger age groups whose mental health was significantly affected during the UK lockdown.
- The quick read: what you need to know
- Mental health, wellbeing, and Covid-19
- Covid-19 worries and experiences affect mental health
- Sources of stress
- Depression and anxiety fell during lockdown, but may be rising now
- How Covid-19 has affected groups differently
- Implications for a wellbeing-based recovery
Downloads
Downloads
![]()
[gravityform id=1 title=true description=true ajax=true tabindex=49]

