Understanding the experience of terminal illness in working-age people
We partnered with Marie Curie, the UK’s leading charitable funder of palliative and end of life care research, to better understand the experience of terminal illness in working-age people. The project focused on mental health and wellbeing, and the role of employer support.
Here the Centre’s Head of Implementation, Joanne Smithson, and Marie Curie’s Research Officer Izzie Baverstock-Poppy, discuss the project, its insights and what this means for business and decision makers.
Identifying a gap in the evidence
There is evidence of strong bi-directional links between wellbeing and employment: being employed and having access to good work can improve your wellbeing, and having good wellbeing can make it easier to work. However, people of working age who have been diagnosed with a terminal illness, and those who care for them, often find themselves forced to leave their employment.
There is a gap in research looking at working age people’s experiences of terminal illness. There are no official figures on the number of working age people living with a terminal diagnosis, and there is very little information on the employment policies and practices designed to support them.
The Special Rules for End of Life bill received Royal Assent last month, making it easier for terminally ill people to claim benefits. This will help reduce inequality in wellbeing, and support the 25,000 people a year of working age who die whilst in poverty. However, our research shows there is so much more we can do.
What we did
The What Works Centre for Wellbeing partnered with Marie Curie to collate what is known and what is needed to most effectively support people of working age living with a terminal illness.
This included:
- designing and commissioning a scoping review of peer-reviewed and grey literature to understand what is currently known about the experiences of terminally ill people of working age;
- conducting a survey of over 1,000 HR professionals to identify policies and practices currently in place designed to support employees working with a terminal illness diagnosis;
- issuing a ‘Call for Practice’ to curate practice examples from organisations and communities of care which offer support to people with a terminal illness diagnosis who want to continue to work.
Key findings
Scoping review
The scoping review synthesised six papers. Only one study was published within the last five years, and only one was from the UK, indicating a significant evidence gap.
The review identified three core and inter-related themes (figure 1), along with a separate theme of factors affecting continuation of work.
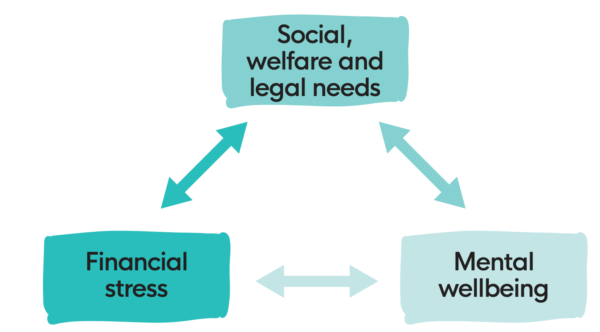
Fig. 1
The findings indicate that people of working age experience significant financial and legal challenges as a direct result of terminal illness. This can interact with challenges of their diagnosis and compound the poor mental wellbeing of individuals and their close family members.
We found evidence that factors unique to this age group, such as loss of family income, cost of childcare, and mortgage and rent costs, may cause additional strain compared to older populations. We found evidence that the financial stress experienced by this group of people can vary depending on individual characteristics which suggests inequalities by gender, ethnicity, and costs of healthcare.
There was little exploration of the benefits to mental wellbeing gained by continuing to participate in work. When exploring the range of quantitative measures used to assess health at the end of life, there were several objective and subjective measures of physical health and health care used, but very little focus on emotions, mental health, and wellbeing.
Survey of HR Decision Makers
The survey revealed:
- Over a third of respondents (35%) said their company had experience supporting a terminally ill employee.
- The most common support provided by companies was flexible working, work adjustments and paid time off, with less than half of companies managing an employee’s terminal illness outside of standard sickness reporting processes (figure 2).
- Almost half of respondents (44%) said their organisation had policies in place for terminally ill employees.
- Of these existing policies, two thirds formed part of a wider company policy (68%); the rest were stand-alone policies (32%).
- Policies were more likely to be found in larger companies (60%) than smaller organisations (33%) (figure 3).
- Policies were more common in companies within the financing and accounting industry (51%) as well as the IT and telecoms industry (56%).
- Policies were less likely to be in place in companies in hospitality and leisure (27%).

Fig. 2 – percentage frequency of support measures by type
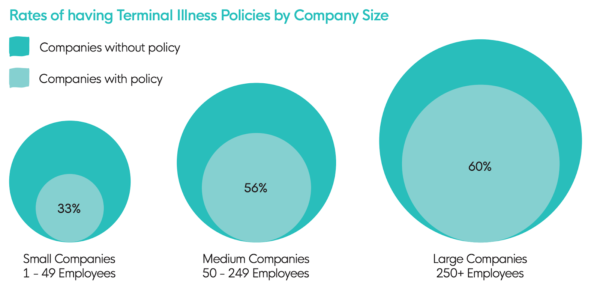
Fig. 3
Ultimately, we uncovered an ‘employer lottery’ in which the support people receive varies significantly.
There are pockets of great practice, but too often employees are likely to find themselves unclear on the support available and unsure of how to access it. In some cases, this ‘employer lottery’ is further compounded by value judgements, which could, in the absence of published procedures, lead to unjust and avoidable inequity in support.
A detailed discussion of methods and findings for the review and survey is available in the project overview and full report.
Impact
We co-presented a roundtable at the House of Lords on Tuesday 22nd November 2022. Hosted by Lord Gus O’Donnell, the event brought together people with lived experience, key stakeholders, employers, parliamentarians and policy professionals to inspire change.
The project is already having an impact within Marie Curie. The charity is using the research findings to support the updating of their Terminal Illness Policy, which will give guidance to managers on effectively managing and supporting employees who are terminally ill.
“We have been able to review our internal policy alongside the report recommendations, with the aim of ensuring our employees are treated with the right sensitivity, flexibility and compassion. The report highlighted four key areas: social, welfare and legal needs, financial needs, mental wellbeing needs and factors affecting decisions to work. These have been especially beneficial when structuring our thinking.” – Jill Pollard, Policy Lead in People Team, Marie Curie
The charity is also exploring ways to support HR professionals to review their companies policies around terminal illness.
If you are interested in attending a workshop for HR leads reviewing organisation policy to support people working with a terminal illness, please contact joanne.smithson@whatworkswellbeing.org
What’s next?
For evidence-informed policy making we need real-world insights and more high-quality information around effective employment policies and practices.
This can be achieved by:
- reviewing national employment legislation to ensure appropriate safeguards, reasonable adjustments and support are in place to protect terminally ill workers;
- preparing guidance on minimum standards and good practice for large, medium-sized and small employers, across all industries and sectors;
- brokering collaborations between HR professionals and occupational health services to develop effective frameworks to support employees with a terminal diagnosis.
HR professionals highlighted:
- the importance of a trusted, compassionate workplace culture;
- having outline policies and procedures in place to guide early discussions;
- a need for improved guidance and training resources.
It would be beneficial for future research to:
- explore personal motivations to work in the context of a limited life expectancy;
- understand how and why experiences at work for people with terminal illness vary;
- assess the effectiveness of interventions for supporting employees with a terminal illness.
Join us on Thursday 12 January 2023, 14:00-15:30 GMT online to discuss the findings and implications in more detail. The virtual event will include presentations, a selection of breakout sessions, and an opportunity for audience questions.
